Hall M, Hornung R, Chevrier J, Ayotte P, Lanphear B, Till C - "Fluoride Exposure and Thyroid Hormone Levels in Pregnancy: The MIREC Cohort" Environment International 108442 (2024)
https://doi.org/10.1016/j.envint.2024.108442
Abstract
Background
Fluoride exposure may increase the risk of hypothyroidism, but results from previous studies are inconsistent at low-level fluoride exposure (i.e., ≤ 0.7 mg/L). Human studies of fluoride and thyroid hormone levels in pregnancy are scarce.
Objectives
We examined associations between fluoride exposure and maternal thyroid hormone levels in a Canadian pregnancy cohort, with consideration for fetal sex-specific effects.
Methods
We measured fluoride concentrations in drinking water and spot urine samples collected during each trimester from 1876 pregnant women enrolled in the Maternal-Infant Research on Environmental Chemicals (MIREC) study. We also measured maternal thyroid stimulating hormone (TSH), free thyroxine (FT4), and total thyroxine (TT4) levels during the first trimester of pregnancy. We used linear and non-linear regression models to estimate associations between fluoride exposure and levels of TSH, FT4, and TT4. We explored effect modification by fetal sex and considered maternal iodine status as a potential confounder.
Results
A 1 mg/L increase in urinary fluoride was associated with a 0.30 (95%CI: 0.08, 0.51) logarithmic unit (i.e., 35.0%) increase in TSH among women pregnant with females, but not males (B=0.02; 95%CI: -0.16, 0.19). Relative to women with urinary fluoride concentrations in the first quartile (0.05-0.32 mg/L), those with levels in the third quartile (0.49-0.75 mg/L) had higher FT4 and TT4 (i.e., inverted J-shaped associations), but the association was not statistically significant after adjustment for covariates (p= 0.06). Water fluoride concentration showed a U-shaped association with maternal FT4, whereby women with water fluoride concentrations in the second (0.13-0.52 mg/L) and third (0.52-0.62 mg/L) quartiles had significantly lower FT4 compared to those with levels in the first quartile (0.04-0.13 mg/L). Adjustment for maternal iodine status did not change the results.
Discussion
Fluoride exposure was associated with alterations in maternal thyroid hormone levels, the magnitude of which appeared to vary by fetal sex. Given the importance of maternal thyroid hormones for fetal neurodevelopment, replication of findings is warranted.
2024: Fluoride Exposure and Thyroid Hormone Levels in Pregnancy: The MIREC Cohort
-
pfpcnews
- Posts: 1006
- Joined: Mon Apr 03, 2006 5:50 am
-
admin
- Site Admin
- Posts: 5517
- Joined: Tue Jan 18, 2005 10:25 pm
Question 1: Iodine Status
NOTE 01/22/2024: The results of the new study by the York/MIREC team (Hall et al., 2024) do NOT show adverse effects of fluoride, as claimed by some in the anti-fluoridation movement. The small and limited effects observed are entirely in line with observed fluoride effects in humans or animals exposed to elevated iodine levels, also documented in the decades-long use of fluoride in the treatment in iodine-induced hyperthyroidism. For example, in hyperthyroid patients, any increase in TSH and a decrease in FT4 would be seen as markers that treatment is working. In that case, such results would be seen as a benefit.
However, once again it is of utmost importance to recognize that excess iodine ingestion itself may also cause an increase in TSH and a decrease in FT4 levels, as a result of iodine-induced thyroid dysfunction, commonly observed in pregnant women consuming too much iodine. This is also observed in children exposed to excess iodine (Lee et al., 2023).
It is beyond time for the York/MIREC team to accurately and properly address this issue.
It is crucial to examine iodine/thyroid status when evaluating fluoride toxicity in pregnant women and their offspring. Both mother and fetus exhibit heightened sensitivity to even slight alterations in thyroid hormone metabolism.
Fluoride toxicity depends on the individual's iodine/thyroid status.
1. Adjustment for Maternal Iodine Status
QUESTION: The authors claim that they adjusted for maternal iodine status. Is this true?
ANSWER: No. They did not. Not in this study, nor have they ever done so in the past - although claiming that they did.
Once again, they merely considered iodine "sufficiency" - or their own interpretation of such - and compared to "insufficiency".
"Insufficiency" is certainly not the problem here.
As shown below, the concerns have to do with iodine intake that is too high, normally categorized as "more-than-adequate" or "excessive".
As discussed elsewhere, this is due to the high iodine intake from the prenatal supplements. [88% of the pregnant women in the MIREC cohort took prenatal supplements containing approx. 220 µg of potassium iodide, resulting in an average iodine intake of 452 μg/day (Krzeczkowski et al., 2023). The WHO recommendation for pregnancy is 250 μg/day.]
"Iodine status" during pregnancy is divided into four categories, based on urinary iodine concentrations (UIC):
The full range of iodine intake levels needs to be considered, as excessive iodine intake may impact thyroid function just like iodine deficiency.
It is well-established that the correlation between alterations in thyroid function and urinary iodine levels follows a U-shaped curve:
However, the York team continually offers misleading information on this issue.
Here, the authors write:
Further, neither Griebel-Thompson et al. (abstract only) nor Malin et al. (Till's team) ever considered "more-than-adequate" or "excessive" iodine intake.
In fact, that was made quite clear by Malin et al. who had removed all participants with excessive iodine intake from their study:
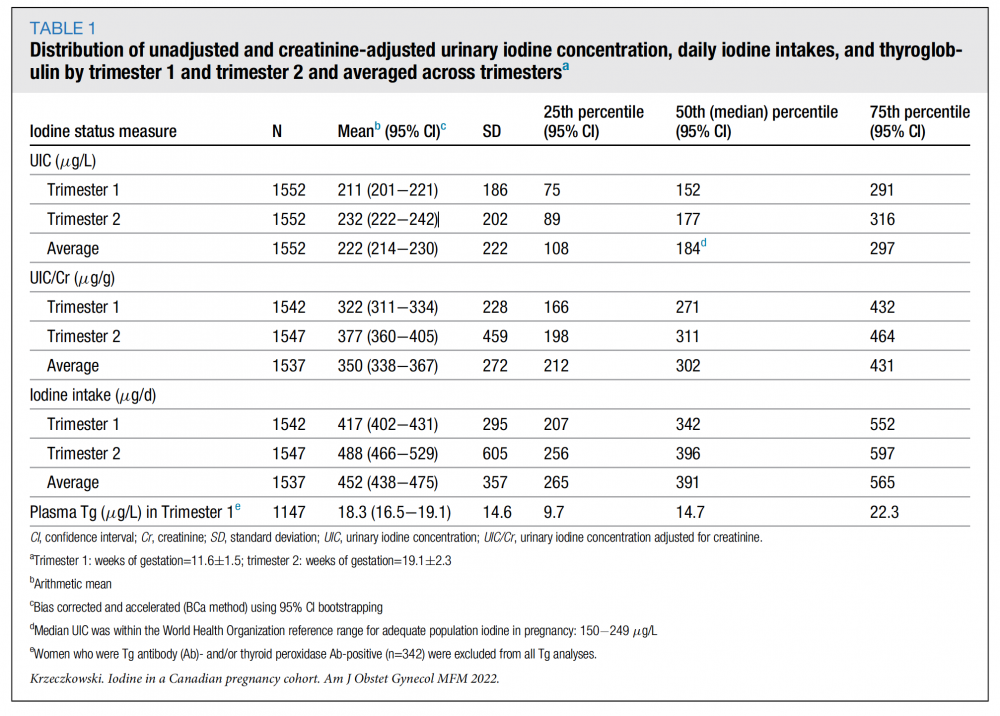
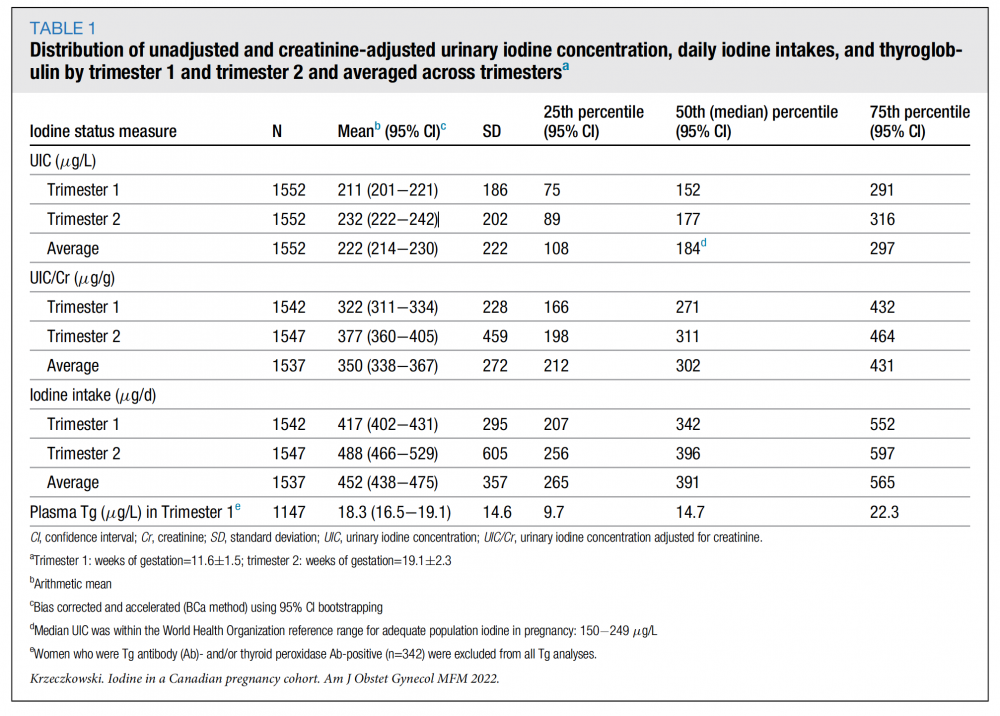
Secondly, they seem to not understand their own findings. The Krzeczkowski (York team) paper showed that at least 25% of the women had a UIC of >250 μg/L, indicating more-than-adequate iodine status. When using the creatinine-adjusted UIC (UIC/cr), the majority of women had "more-than-adequate" intake levels. When relying on daily iodine intake estimates, almost all women exceeded the WHO-recommended levels (250 μg/day).
Here is Table 1 from Krzeczkowski et al., 2023:
To appreciate the significance of this, it's crucial to understand that a maternal UIC exceeding 250 μg/L has been linked to:
The lack of awareness on iodine needs and thyroid hormone metabolism during gestation is evident in many papers by the Till team. For instance, in Goodman et al. (2022), the team defined their own "adequate" range for iodine intake, based on a WHO document applicable to typical adults, which is inappropriate for pregnant women. In that study, they claimed a UIC/cr of 200-600 μg/g to be reflective of "adequate" iodine status (!).
This ignorance has led to numerous modelling errors and misinterpretations, and questionable methods overall.
For example, thyroglobulin (Tg) levels were investigated as an indicator for iodine sufficiency. While Tg levels might be an adequate replacement for taking UIC measurements in iodine-deficient populations, they have only very limited use during pregnancy, or in cases of excessive iodine ingestion. Hence, many experts have advised against using Tg levels to determine iodine status during pregnancy (i.e. Laurberg et al., 2007; Koukkou et al., 2006).
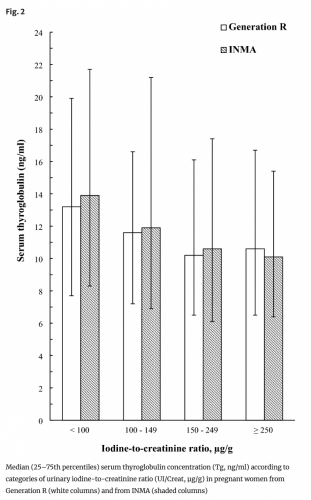
As one can tell from Fig. 2 of the Dineva study - cited by Hall - Tg levels do not differentiate between adequate (UIC/cr 150-249 μg/g) and more-than-adequate intake (UIC/cr >250 μg/g).
REFERENCES
All references cited are listed on the "York/MIREC - FAQ References" page:
viewtopic.php?f=97&t=5022
However, once again it is of utmost importance to recognize that excess iodine ingestion itself may also cause an increase in TSH and a decrease in FT4 levels, as a result of iodine-induced thyroid dysfunction, commonly observed in pregnant women consuming too much iodine. This is also observed in children exposed to excess iodine (Lee et al., 2023).
It is beyond time for the York/MIREC team to accurately and properly address this issue.
It is crucial to examine iodine/thyroid status when evaluating fluoride toxicity in pregnant women and their offspring. Both mother and fetus exhibit heightened sensitivity to even slight alterations in thyroid hormone metabolism.
Fluoride toxicity depends on the individual's iodine/thyroid status.
1. Adjustment for Maternal Iodine Status
QUESTION: The authors claim that they adjusted for maternal iodine status. Is this true?
ANSWER: No. They did not. Not in this study, nor have they ever done so in the past - although claiming that they did.
Once again, they merely considered iodine "sufficiency" - or their own interpretation of such - and compared to "insufficiency".
"Insufficiency" is certainly not the problem here.
As shown below, the concerns have to do with iodine intake that is too high, normally categorized as "more-than-adequate" or "excessive".
As discussed elsewhere, this is due to the high iodine intake from the prenatal supplements. [88% of the pregnant women in the MIREC cohort took prenatal supplements containing approx. 220 µg of potassium iodide, resulting in an average iodine intake of 452 μg/day (Krzeczkowski et al., 2023). The WHO recommendation for pregnancy is 250 μg/day.]
"Iodine status" during pregnancy is divided into four categories, based on urinary iodine concentrations (UIC):
- Insufficient: UIC <150 μg/L
- Adequate: UIC 150-249 μg/L
- More-than adequate: UIC 250-499 μg/L
- Excessive: UIC >500 μg/L
The full range of iodine intake levels needs to be considered, as excessive iodine intake may impact thyroid function just like iodine deficiency.
It is well-established that the correlation between alterations in thyroid function and urinary iodine levels follows a U-shaped curve:

Image taken from Ma et al., 2022. SEE full graph: https://www.nature.com/articles/s41467- ... /figures/4
However, the York team continually offers misleading information on this issue.
Here, the authors write:
Again, this is entirely misleading, implying that other iodine states had been investigated."Controlling for maternal urinary iodine status in all models of fluoride exposure and maternal thyroid hormone levels did not change the results. Iodine is an essential nutrient for thyroid hormone synthesis and plays an important role in determining the magnitude of fluoride’s effect on the thyroid. Specifically, iodine has been found to modify the association between urinary fluoride concentration and TSH levels among pregnant women (Griebel-Thompson, 2022) and non-pregnant adults, (Malin et al., 2018) such that this association was only significant among those who were classified as iodine insufficient."
Further, neither Griebel-Thompson et al. (abstract only) nor Malin et al. (Till's team) ever considered "more-than-adequate" or "excessive" iodine intake.
In fact, that was made quite clear by Malin et al. who had removed all participants with excessive iodine intake from their study:
The ignorance is further displayed in the statement that follows:"We removed these participants because excess iodine levels can cause abnormalities in TSH (Katagiri et al., 2017), including elevations, and we wanted to test the relationship between fluoride exposure and TSH as a function of iodine deficiency, not iodine excess." (Malin et al., 2018)
So - the authors did not specifically investigate whether the relationship between fluoride exposure and thyroid hormones varied based on different levels of maternal iodine intake."Effect modification was not tested directly in the current study due to limited statistical power given nearly all women in the MIREC cohort were classified as iodine sufficient in a prior study (Krzeczkowski, 2023) based on our estimate of daily iodine intake."
Secondly, they seem to not understand their own findings. The Krzeczkowski (York team) paper showed that at least 25% of the women had a UIC of >250 μg/L, indicating more-than-adequate iodine status. When using the creatinine-adjusted UIC (UIC/cr), the majority of women had "more-than-adequate" intake levels. When relying on daily iodine intake estimates, almost all women exceeded the WHO-recommended levels (250 μg/day).
Here is Table 1 from Krzeczkowski et al., 2023:
To appreciate the significance of this, it's crucial to understand that a maternal UIC exceeding 250 μg/L has been linked to:
- Subclinical hypothyroidism (SCH) (Corcino et al., 2019; Shi et al., 2016; Wang et al., 2017; Liu et al.,; Sang et al., 2012; Yang et al., 2020)
Maternal SCH in pregnancy is associated with increased risk of adverse neonatal outcomes, including delayed intellectual and motor development, low birth weight, premature delivery, fetal distress and fetal growth restriction.
- Gestational diabetes and hypertensive disorders (Silva de Morais et al., 2020)
- Non-immune hypothyroidism (Kim et al., 2019)
- Increase in thyroid auto-immune disease (TPOAb) (Habimana et al., 2014; Shi et al., 2016)
- Loss of IQ in offspring (Carvalho et al., 2022)
- Macrosomia (LGA) (Dong et al., 2021)
- Thyroid nodules (Gao et al., 2021; 2019)
The lack of awareness on iodine needs and thyroid hormone metabolism during gestation is evident in many papers by the Till team. For instance, in Goodman et al. (2022), the team defined their own "adequate" range for iodine intake, based on a WHO document applicable to typical adults, which is inappropriate for pregnant women. In that study, they claimed a UIC/cr of 200-600 μg/g to be reflective of "adequate" iodine status (!).
This ignorance has led to numerous modelling errors and misinterpretations, and questionable methods overall.
For example, thyroglobulin (Tg) levels were investigated as an indicator for iodine sufficiency. While Tg levels might be an adequate replacement for taking UIC measurements in iodine-deficient populations, they have only very limited use during pregnancy, or in cases of excessive iodine ingestion. Hence, many experts have advised against using Tg levels to determine iodine status during pregnancy (i.e. Laurberg et al., 2007; Koukkou et al., 2006).
As one can tell from Fig. 2 of the Dineva study - cited by Hall - Tg levels do not differentiate between adequate (UIC/cr 150-249 μg/g) and more-than-adequate intake (UIC/cr >250 μg/g).
- High iodine intake was found to be the main cause of thyroid dysfunction among pregnant women. The prevalence of excessive iodine intake in 10,736 pregnant women in different regions of the world was 52%. (Candido et al., 2023).
- In light of recent large-scale studies showing an increase in subclinical hypothyroidism when maternal UIC is greater than 250 μg/L, calls have been made advocating that an upper level of sufficiency in pregnancy should not exceed an intake of 250 µg/day (Lee & Pearce, 2015; Shi et al., 2016).
REFERENCES
All references cited are listed on the "York/MIREC - FAQ References" page:
viewtopic.php?f=97&t=5022